Whether your first period (or menarche) was greeted with grief or celebration, learning to live with (or at least coexist with) your menstrual cycle can be a years- or decades-long journey. This guide will provide with frankly, way more information than you need to exist as a menstruating human on this planet (I learned a lot while doing my research), but our aim is to arm you with literally any and all the information you could possibly need to start working with your period, instead of against it.
The Menstrual Cycle
The average girl will begin their period at or around 12 years of age and will have a menstrual cycle until they are 51 years old… that’s 39 years of periods! If your period lasts between 4-8 days (which is the average length of a period), that means that in your lifetime you could be actively menstruating for anywhere between over 5-10 years of your life. You’d think with that kind of time commitment, we would’ve been taught all about the intricacies of our menstrual cycles!
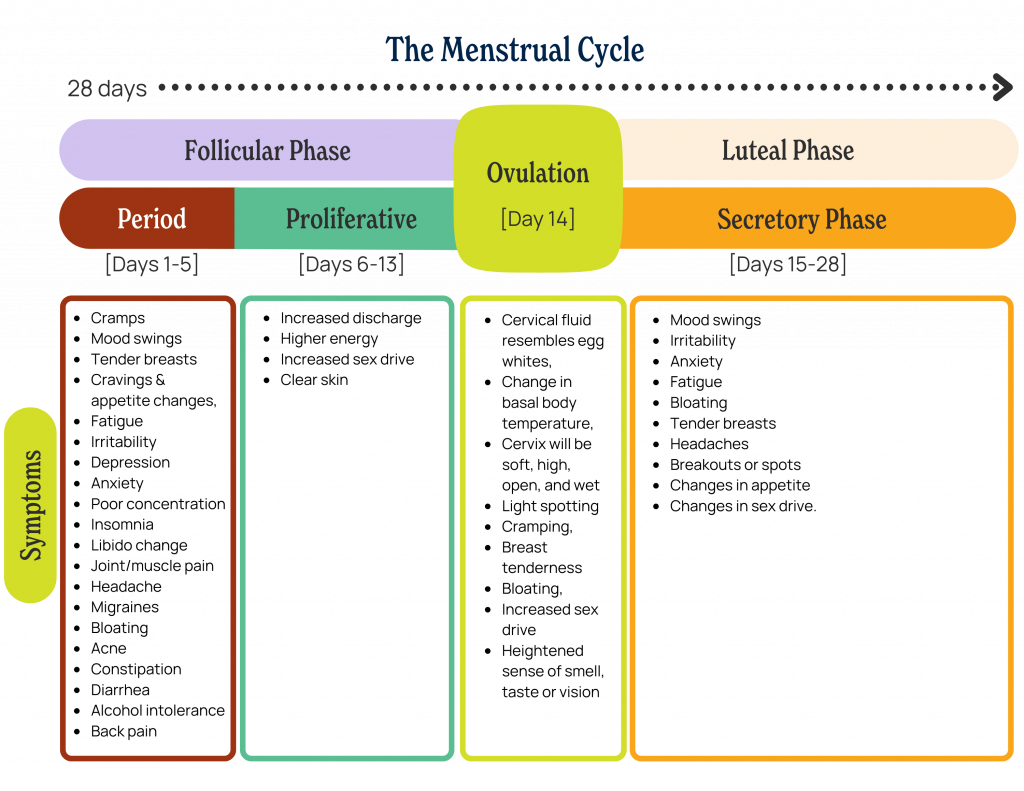
The menstrual cycle, which lasts 24-38 days for the average menstruating adult, is organized by the ovarian cycle, then further organized by uterine cycle stages. The days leading up to ovulation which happens in the middle of the cycle are referred to as pre-ovulation, or the follicular phase; the fourteenth day of the cycle is ovulation; the days following ovulation (until the conclusion) of the cycle are referred to as post-ovulation, or the luteal phase. Below is an outline of the menstrual cycle based on a 28-day-long cycle.
Pre-ovulation (Follicular Phase)
The follicular phase occurs during days one through thirteen as the period ends during which the ovary prepares to release an egg initiating a new menstrual cycle.
Menstruation
The period occurs between days one through five of the cycle when your levels of estrogen and progesterone are low. During the period, The uterus sheds the endometrial lining that has built up throughout the last cycle and the pituitary gland in the brain that produces hormones creates follicle-stimulating hormone (FSH), which communicates to the ovaries that they should prepare an egg (follicle).
A typical period is considered the shedding of between 5-80 mL of blood and tissue, which is up to about six tablespoons. An average person usually sheds about 35-40 mL of blood and tissue during their period – anyone who sheds more than this may be considered to have heavy menstrual bleeding. It’s good to monitor how heavy your flow is because long periods of heavy bleeding can be concerning and even lead to anemia. It is very common to notice clumps of tissue in menstrual blood and see variations in the coloring of menstrual blood.
Proliferative Phase
During the proliferative phase (days six through thirteen), the uterine lining (endometrium) builds up again after being shed during menstruation. The endometrial lining is where a fertilized egg would have attached/will attach in the case of a pregnancy. During this phase, the cervix may appear more dilated and you may notice increased amounts of vaginal discharge – both of which are normal.
Ovulation
Did you know that the frequency of ovulation has changed over time and varies based on contraceptive use, time spent pregnant/breastfeeding, nutrition, chronic illness, stress, jet lag, smoking, socioeconomic status, and much more? Apparently, “in the [global north], we ovulate roughly 400 times throughout our lifespan,” but “prehistorically, women would have ovulated less than half as often.”
Ovulation falls in the middle of the cycle – on day fourteen of a 28-day cycle – and is the point when the egg is released from the ovary into the fallopian tube. Just before ovulation, estrogen levels rise and then drop shortly after the egg is released. This rise in estrogen levels (emitted by the follicle that is to release an egg) is what triggers the creation of luteinizing hormone, which then triggers the release of the egg (follicle).
If you are trying to get pregnant–or trying not to–it can be quite helpful to know the ins and outs of ovulation. As discussed above, we know that ovulation happens in the middle of a cycle when the dominant follicle releases its egg (a few follicles are developing at any given time, so the one that is more mature or ‘ready’ is the dominant one), then after traveling to the fallopian tube where the egg has around 12-24 hours to be fertilized. If the egg does become fertilized, “it travels to the uterus over the following 6–12 days, to possibly implant for pregnancy.”
‘How do I know if I’m ovulating?’
Primary symptoms of ovulation include a change of cervical fluid to the consistency of egg whites, changes in basal body temperature, and the cervix will be soft, higher up, open, and wetter. Secondary symptoms that may be more noticeable to you include light spotting, cramping, breast tenderness, bloating, an increased sex drive, and a heightened sense of smell, taste, or vision.
During adulthood, you are likely ovulating if you have a regular cycle, but a few ways to check are to: track your cycle, use over-the-counter ovulation urine tests, track your cervical fluid and basal body temperature, have a healthcare provider check your hormonal profile via a blood test.
Ovulation Tests
Ovulation tests can be purchased at your local pharmacy or online. It is said that tests can be taken at any time of the day, but taking them at the same time each day is best. These tests check your levels of luteinizing hormone (LH) which peaks right before ovulation.
Look for products like Stix Ovulation Tests (7 tests for $17) that are over 99% accurate and you take the test 12 days after the start of your last period.
Physical Signs: Cervical Mucus and Basal Body Temperature
A common natural way of tracking fertility is through tracking cervical mucus and Basal Body Temperature (BBT). As aforementioned, during ovulation, cervical fluid is likely to be more like the consistency of egg whites.
During the latter part of your menstrual cycle, the body’s resting temperature increases, and tracking these temperature changes can help you know when you are ovulating and most fertile. The average person’s body temperature usually falls between 97°F (36.1°C) to 99°F (37.2°C) but varies from person to person – BBT tends to be a bit lower during the follicular phase and rises then plateaus during the luteal phase in response to the release of progesterone.
Clue recommends the following as guidelines for monitoring BBT:
- Take temperature immediately after waking, while laying still in bed, before sitting upright
- Take it every day, at the same time
- Use a special thermometer with 0.10-degree accuracy for Fahrenheit (ºF) and 0.01-degree for Celsius (ºC), for precise rounding
- Make note of which days are “unreliable” due to environmental factors, such as changes in sleep patterns, disturbed or shortened sleep, jet lag, heavy drinking, illness, or medications, which can cause changes to your menstrual cycle
- See a doctor if you have a fever for longer than 48–72 hours, or have a fever that stays at or increases from 103˚F (39.4˚C) or suspect that you are pregnant
Post-ovulation (Luteal Phase)
The luteal phase (days fifteen to twenty-eight) is the time between ovulation and menstruation and is also when the body is preparing for a possible pregnancy. During this phase, progesterone levels peak and then drop before menstruation – this is a result of the follicle that held the egg becoming what is called the corpus luteum, which if fertilized, would support the pregnancy in its earliest stages.
If you’ve ever wondered what an ovarian cyst is, it is sometimes related to the corpus luteum, as most ovarian cysts are a result of normal processes that occur during the menstrual cycle. If the follicles (that would eventually become a corpus luteum) that hold eggs continue to keep growing, it becomes a functional cyst, of which there are two types: follicular cysts and corpus luteum cysts. When a follicle doesn’t rupture or release its egg and it continues to grow, it becomes a follicular cyst. When a follicle releases its egg and then accumulates fluid, it becomes a corpus luteum cyst. You may not know if you have a cyst, though if one ruptures, you may have moderate to severe abdominal pain, fever, or vomiting and you should seek immediate medical attention – you may mistake it for appendicitis.
Secretory Phase
The secretory phase follows ovulation and lasts until the start of the next period and during this phase, “the lining of the uterus releases or secretes chemicals that will either help an early pregnancy attach if an egg was fertilized, or help the lining break down and shed if no egg was fertilized.” Basically, the endometrium is gearing up to either (A) support a pregnancy or (B) shed during the next period. The endometrium stops thickening due to the increased levels of progesterone and the endometrium produces and secretes (hence the name ‘secretory phase’) chemicals like prostaglandins (which are a primary cause of menstrual cramps). In addition to cramps, it is during this phase (often during the one to two weeks prior to menstruation) that many people experience Premenstrual Syndrome, or PMS.
Tracking Your Cycle
Whether you are trying to plan ahead for a vacation, hoping to get pregnant, or trying to wear white at an upcoming event, it is helpful to know where you stand with your cycle. When you track your cycle, the Mayo Clinic recommends monitoring the following:
- End date: How long does your period typically last? Is it longer or shorter than usual?
- Flow: Record the heaviness of your flow. Does it seem lighter or heavier than usual? How often do you need to change your sanitary protection? Have you passed any blood clots?
- Abnormal bleeding: Are you bleeding in between periods?
- Pain: Describe any pain associated with your period. Does the pain feel worse than usual?
- Other changes: Have you experienced any changes in mood or behavior? Did anything new happen around the time of change in your periods?
Clue App
The period tracking app that I personally use and trust is Clue, which is “a period tracking app, a trusted menstrual health resource, and a thought leader in femtech. By combining science and technology, [they] are actively changing the way people learn, access, and talk about menstrual and reproductive health around the world.” You can input your cycle, symptoms, fertility efforts, sexual activity, and more into the app and even the free version will very accurately predict your cycle based on precedent.
One of the concerns that many people share in our political climate is privacy regarding our reproductive health. In response to these concerns, the Clue Co-CEOs published the following privacy statement to reassure users:
“We have received messages from our American users concerned about how their tracked data could be used by US courts if Roe vs Wade were overturned. As the female Co-CEOs of Clue, we promise you that we will never turn your private health data over to any authority that could use it against you. Your personally identifiable health data regarding pregnancies, pregnancy loss or abortion, is kept private and safe.”
Me, Myself, and My (PMS)
Unfortunately, females are all too familiar with the discomfort, pain, and annoyances that come with menstrual cycles… chocolate cravings, anyone? Where roughly 80% of females report at least mild premenstrual symptoms, anywhere from 20% to half of females report moderate-to-severe premenstrual symptoms. The Mayo Clinic divides PMS symptoms into two categories: Emotional and behavioral signs and symptoms and Physical signs and symptoms.
Emotional and behavioral symptoms of PMS include: tension or anxiety, depressed mood, crying spells, mood swings and irritability or anger, appetite changes and food cravings, trouble falling asleep (insomnia), social withdrawal, poor concentration, and change in libido (increase or decrease).
Physical symptoms of PMS include: joint or muscle pain, headache, fatigue, weight gain related to fluid retention, abdominal bloating, breast tenderness, acne flare-ups, constipation or diarrhea, cramping (dysmenorrhea), and alcohol intolerance.
Cramps Really Cramp My Style
One of the biggest complaints (justifiably so) about PMS and menstruation is menstrual cramps. Some people don’t experience cramps, some people have to curl up into a ball and wait for them to pass for a few days each month. What are menstrual cramps, you ask? In order to shed the uterine lining, the uterus contracts to push it out through the cervix into the vaginal canal. These uterine contractions are what is felt as a ‘cramp.’
Common treatments for cramps include OTC pain medication, TENS devices, heat packs, magnesium supplements, and one of the best treatments is actually orgasms! For pain management products, reference the end of this blog.
Menstruation Nation
Clue surveyed over 4,000 users about their PMS and menstrual symptoms and some commonly reported ailments include acne, headache, dizziness, or lightheadedness, fatigue, weight changes, fatigue, cold hands/feet, backache and/or leg pain, chronic pelvic pain, diarrhea or nausea, constipation, painful bowel movements, brittle nails and/or hair loss, pale skin, fast heartbeat and/or shortness of breath, experience watery, bloody or foul-smelling vaginal discharge, experience frequent urination and/or difficulty urinating, experience excessive hair growth, experience chest pain, pain and/or bleeding during or after sexual intercourse.

The graph represents the % of the 4,000 users surveyed who reported each PMS symptom.
Abnormal Menstrual Cycles
For some people, PMS symptoms are actually incredibly debilitating and affect their quality of life – this can be a sign of something more serious that you should address with a healthcare provider. Remember: some amount of PMS symptoms are normal, but there’s you shouldn’t have to suffer in silence. Your HCP may be able to help you figure out pain/symptom management or work with you to investigate more serious problems that may be going on (some of which are outlined below).
Pregnancy or Breastfeeding
There is no cause for concern if you do not have a period during pregnancy or while you are breastfeeding. During pregnancy, the endometrial lining that would shed during menstruation is actually being used to supply oxygen and nutrients and to protect the embryo (and later, fetus), thus you do not menstruate, or shed this lining.
Depending on how frequently/regularly you are breastfeeding a baby, you may not get your period at all until you stop breastfeeding altogether. This is because “the hormone that causes you to make milk, prolactin, also stops you from ovulating and having your period.” If you reduce the amount you breastfeed or stop, your period is likely to return. However, the return of your period should not drastically affect your milk supply. This also means that while breastfeeding, if you are not ovulating, you are not going to become pregnant. If, while breastfeeding, you experience irregular periods, you should consult your doctor.
Eating disorders, extreme weight loss, or excessive exercising
In order for the body to carry out its normative functions, like walking, talking, breathing, and menstruating, it needs the proper fuel. Amenorrhea (when menstruation ceases for over three months) and oligomenorrhea (irregular and/or inconsistent menstruation) are both causes for concern in those with eating disorders and in those who exercise excessively and this should be immediately addressed with a healthcare provider.
Anorexia Nervosa, Bulimia Nervosa, & Compulsive Exercise
These three eating disorders are characterized by insufficient nutrition by lack of consumption, purging, or excessive exercise after eating and all affect the menstrual cycle by way of amenorrhea.
Primary Amenorrhea
If restrictive eating habits begin prior to puberty, this can delay the onset of a person’s first menstrual cycle. This is called primary amenorrhea.
Secondary Amenorrhea
For those who had previously menstruated, but due to malnutrition or excessive exercise their menstrual cycle stopped, this is called secondary amenorrhea.
Binge Eating Disorder
A study from 2013 found that “Women who reported lifetime binge eating were more likely to report either amenorrhea or oligomenorrhea than women who reported no binge eating.”
Binge Eating Disorder (BED) is described by NEDA as “recurrent episodes of eating large quantities of food (often very quickly and to the point of discomfort); a feeling of a loss of control during the binge; experiencing shame, distress or guilt afterward; and not regularly using unhealthy compensatory measures (e.g., purging) to counter the binge eating.”
The previously mentioned study believes that this correlation between BED and menstrual irregularity may be due to metabolic and endocrinological factors.
Functional Hypothalamic Amenorrhea (FHA)
FHA can occur when there is extreme and/or chronic nutritional deficiency. It is a result of inadequate energy intake combined with high energy output and as a 2016 study reports, it results in, among other alterations, changes in hormonal capacities. Specifically, it results in the suppression of luteinizing hormones that are required for ovulation. FHA also “alters the production of estrogen and progesterone resulting in subclinical or clinical menstrual dysfunction.”
Sexually Transmitted Infections (STIs)
Some STI symptoms may mimic menstrual symptoms, while others may affect your actual menstrual cycle. For example, gonorrhea may cause bloody discharge, heavy menstrual bleeding, breakthrough bleeding (bleeding between periods), discomfort during urination, and painful bowel movements – all of which are PMS symptoms. Chlamydia can cause discomfort during urination, pain during sex, and breakthrough bleeding/spotting – which could be confused for PMS. Though many females don’t have obvious symptoms of STIs if they do have them, that’s why it’s important to get tested regularly. “For people with herpes,” sex educator Christina Tesoro explained to HelloFlo, “some are more likely to have an outbreak during their period, though this isn’t true for everyone.” Regarding fertility, undiagnosed and untreated STIs actually are the global leading cause of infertility and this is entirely preventable with diagnosis and treatment.
So, how can you tell if it’s your period or potentially an STI? Watch out for abnormal changes in the color, texture, or smell of your discharge and/or menstrual blood and visit an HCP.
Pelvic inflammatory disease (PID)
This infection of the reproductive organs can cause irregular menstrual bleeding and more than one million people get it every year. PID is a bacterial STI that infects the cervix and is easily treated with antibiotics, however, if untreated, it can spread to the endometrium, fallopian tubes, tissue around the uterus, ovaries, and the lining of the abdomen (peritoneum). Additionally, untreated chlamydia and/or gonorrhea can evolve into PID. Symptoms of PID are usually subtle and you may not be aware of the infection until you are struggling with fertility or develop chronic pelvic pain. When symptoms appear, they often include pain, abnormal/heavy/smelly discharge, breakthrough bleeding, bleeding after sex, pain during sex, fever, and painful/frequent/difficult urination. Long-term complications of untreated PID might include ectopic pregnancy, infertility, chronic pelvic pain, and tubo-ovarian abscess.
Premenstrual dysphoric disorder (PMDD)
Premenstrual dysphoric disorder (PMDD) is, at its core, a more serious form of PMS. The US Office on Women’s Health characterizes it as causing “severe irritability, depression, or anxiety in the week or two before your period starts. Symptoms usually go away two to three days after your period starts.” They also mention that you may need medicine or other treatment to help with your symptoms. PMDD isn’t very common – it only affects about 5% of females who are of reproductive age and many of them may also have anxiety or depression.
The cause of PMDD isn’t known for sure, but it is suspected that the hormonal changes during the menstrual cycle paired with serotonin levels may be at least a partial cause. PMDD is diagnosed by an HCP who will do a physical exam, discuss your health history, ask you to keep a calendar/journal of your symptoms, and to be diagnosed with PMDD, you must have five or more of the eleven symptoms outlined in the Diagnostic and Statistical Manual of Mental Disorders (DSM) and at least one of those reported symptoms “must be depressed mood, anxiety, affective lability or irritability.” PMDD treatments can include antidepressants (continuously or during the luteal phase), ovulation suppression, oophorectomy (removal of one or both ovaries), anti-anxiety medications, birth control pills, OTC pain relievers, stress management, vitamins/minerals/herbs, and/or lifestyle changes.
Polycystic ovary syndrome (PCOS)
The Mayo Clinic defines Polycystic ovary syndrome (PCOS) as “a hormonal disorder common among women of reproductive age. Women with PCOS may have infrequent or prolonged menstrual periods or excess male hormone (androgen) levels. The ovaries may develop numerous small collections of fluid (follicles) and fail to regularly release eggs.” Indications of PCOS often develop at the time of the first menstrual period, but they can appear later in life as well. Some indications of PCOS include irregular periods (infrequent, heavy, or prolonged periods), elevated levels of the male hormone androgen (which can cause excess hair growth, hair loss, and acne), and/or polycystic ovaries (ovaries may be enlarged and follicles may be cystic preventing normative ovulation).
PCOS can affect your menstrual cycle in many ways, making it infrequent, preventing ovulation, causing heavy bleeding, etc. Depending on the person, complications of this condition can (but will not always) include:
- Infertility
- Gestational diabetes or pregnancy-induced high blood pressure
- Miscarriage or premature birth
- Liver inflammation
- Metabolic syndrome — a cluster of conditions including high blood pressure, high blood sugar, and abnormal cholesterol or triglyceride levels that significantly increase your risk of cardiovascular disease
- Type 2 diabetes or prediabetes
- Sleep apnea
- Depression, anxiety, and eating disorders
- Abnormal uterine bleeding
- Cancer of the uterine lining (endometrial cancer)
- Obesity
Endometriosis
Endometriosis is “an often painful disorder in which tissue similar to the tissue that normally lines the inside of your uterus–the endometrium–grows outside your uterus” that affects about 10% of reproductive-age females. The reason that it is often incredibly painful is because like the endometrial lining that is inside the uterus, it thickens and is shed with each period, but it becomes trapped seeing as it has so predetermined path out of the body. When endometrium grows on the ovaries, endometriomas (similar to cysts) can form which can lead to irritation, scar tissue, and adhesions (“bands of fibrous tissue that can cause pelvic tissues and organs to stick to each other”) – eventually, this can affect fertility.
In addition to pain, symptoms include pain during intercourse, painful bowel movements or urination, heavy menstrual bleeding, breakthrough bleeding, infertility, fatigue, diarrhea, constipation, bloating, and nausea.
Treatments include medication (contraceptive steroids, non-steroidal anti-inflammatory medications, and pain killers) and surgery, though the success rates of surgery in decreasing symptoms and increasing the likelihood of pregnancy vary.
Fibroids
Uterine fibroids are growths that develop on the inner walls of the uterus and they can be very small or quite large (even the size of a grapefruit). A person with fibroids may have one or may have many of varying sizes and they can grow over time or pop up quickly. They are not cancerous and cannot become cancerous, but they can cause pelvic pain, heavy menstrual bleeding, breakthrough bleeding, back pain, infertility, painful cramps, pain during sex, prolonged periods, swelling in the uterus or belly, gastrointestinal discomfort, and/or miscarriages, though many people don’t have symptoms at all.
The cause of fibroids is unknown, though genetics, hormones (estrogen and progesterone), diet, Vitamin D deficiency, and stress can be contributing factors. Research has also shown that Black women are more likely to develop fibroids at younger ages – fibroids that grow faster and bigger and cause more severe symptoms.
Premature Ovarian Failure
Premature ovarian failure, or primary ovarian insufficiency (POI), describes the loss of normative ovarian function before the age of forty. A person experiencing POI no longer has their period and can no longer get pregnant. The cause isn’t known 90% of the time, but it can be caused by genetic disorders, a low number of follicles, autoimmune diseases, chemotherapy/radiation therapy, metabolic disorders, or environmental toxins.
Symptoms of POI include hot flashes, night sweats, irritability, poor concentration, decreased sex drive, pain during sex, vaginal dryness, and infertility. POI can potentially put you at risk for anxiety and depression, dry eye syndrome and eye surface disease, heart disease, low thyroid function, and/or osteoporosis.
When to Seek Help
If you have any concerns about your menstrual cycle, you should talk to an HCP or comparable resource. Women’s and females’ pain is often dismissed and you have a human right to the highest degree of health that is attainable. Trust your intuition and your gut (literally) if you think something is wrong, and you can always get a second or third opinion if you aren’t getting the answers you need.
Remember that this blog post is not medical advice nor should it be used as a tool for diagnosis. If you are concerned about something you read in this blog and how it might apply to your health, feel free to print it out or send it to your HCP.
Generally speaking, The Mayo Clinic says that you should consult your health care provider if:
- Your periods suddenly stop for more than 90 days — and you’re not pregnant
- Your periods become erratic after having been regular
- You bleed for more than seven days
- You bleed more heavily than usual or soak through more than one pad or tampon every hour or two
- Your periods are less than 21 days or more than 35 days apart
- You bleed between periods
- You develop severe pain during your period
- You suddenly get a fever and feel sick after using tampons
Working with Your Cycle
Cycle-Syncing
Cycle Syncing, created by Alisa Vitti (women’s Menstrual Health Expert, Functional Nutritionist, and best-selling author of WomanCode), uses the four phases of a menstrual cycle to maximize productivity and lean into the hormonal influences of each phase. While not scientifically proven, adapting your behavior and lifestyle to your body’s natural hormonal changes may allow you to integrate your health into finding a work-life balance.
During Menstruation
During menstruation, your hormones are low and you are able to use analytical and intuitive reasoning to reflect. However, your energy, focus, and productivity will likely be at their lowest. While in this phase, it may be beneficial to cut back on social commitments, get lots of rest, and try not to schedule any big projects or meetings.
During the Follicular Phase
Vitti says that during the follicular phase, your creativity will flourish. During this phase, there is a sharp rise in progesterone and estrogen and a potential rise in testosterone levels, giving you more energy. Now is a great time to be proactive and tackle big projects.
During the Ovulatory Phase
Vitti proposes that communication and collaboration skills are at their best while you are in the ovulatory phase. While you are peaking in estrogen and testosterone, you are likely to feel energetic and proactive, so make social plans and schedule meetings.
During the Luteal Phase
Vitti offers that during the luteal phase, you are most powerful and focused, but you may also be coming down from your hormone high. You might start to feel your productivity dwindle a bit, so start to lighten your workload, take on individual tasks, and prioritize self-care.
Menstruation Myth Busting
Q: Are periods synced to the moon/lunar cycles?
No, they are not. Studies like this one done in 2021 have shown that there is no association between menstrual cycle onset and lunar phases. This is a very popular myth, however.
Q: Is it bad to exercise while I have my period?
Not at all! It may actually help with some of the physical symptoms of PMS.
Q: Can I skip the sugar pill week of my birth control so I can skip my period?
Yes, you can! There is no evidence that it is unhealthy to skip your period. You might experience some breakthrough bleeding, but that’s nothing to be concerned about.
Q: Is it ok to have sex during my period?
Not only is it ok, but it’s actually a great idea! You should still use your normal safer sex products, but there are a few benefits to having sex on your period: extra lubrication, the release of endorphins for a mood boost, relief from cramps and headaches, and the muscle contractions during orgasm might cause your uterus to expel the endometrium faster (making your period end sooner).
Visualizing Your Cycle & the Products that Will Help You Along the Way

MENSTRUAL UNDERWEAR: The Period Company (products start at $12, XS-6X), Modibodi (start at $25, XS-3XL), Bambody (start at $18.90, XS-XXL), Aisle ($32+, gender expansive, 5X-XS). MENSTRUAL CUPS/DISCS: Viv Menstrual Cup ($20), INTIMA Ziggy Menstrual Cup ($44.95), Flex Reusable Disc ($34.99), Nixit Menstrual Cup ($42), Flex Plant+ Disc (12 for $15.99), Flex Disc ($10.99). TAMPONS/PADS: August Build Your Own Period Supply Box (Subscription available, $8.75-$34), Dame Reusable Tampon applicator ($23), Public Goods Organic Cotton Tampons (18 for $4.95), Rael Organic Cotton Pads (16 for $7), Rael Organic Liners (70 for $7), Rael Reusable Pads (3 for $34), Rael Reusable Liners (3 for $30), Marlow Tampon Lubricant ($8.50). DRUG-FREE PAIN RELIEF: Livia ($124), Ovira Noha ($139), Vush Aura ($110), Rael Heating Patches (8 for $16), Abdominal Heating Pad ($49.99). CLEAN UP: Good Clean Love Balance Moisturizing Wash ($11.99), Good Clean Love Rebalance pH-Balanced Wipes ($9.99), Dove Original Beauty Bar (~$2), Dripsticks ($15+). SUPPLEMENTS: Delune Cramp Aid ($19), Delune Steady Mood ($19), Flo PMS ($27+), Semaine PMS & Period Support ($25+), Foria Cramps Be Gone Bundle ($76), Juna Detox Drops ($26+), Calm Stress Relief Gummies ($12+), PYM Mood Chew ($40), Xula Lights Out ($62). MISC: Satisfyer 1 ($34), Fun Factory Lady Bi ($160), Juna Body Oil ($48), Liberator Throw ($99+).
Written by:
Gillian ‘Gigi’ Singer, MPH
American Board Certified Sexologist, Sexuality Educator, and Sex Ed Content Specialist